 The Affordable Care Act (ACA) imposes significant information reporting responsibilities on employers starting with the 2015 calendar year. Employers with 50 or more full time equivalent employees (FTEs), as well as certain employers with fewer than 50 FTEs are subject to the new reporting requirements as of January 1, 2016. The ACA added two new sections to the Internal Revenue Code, Sections 6055 and 6056, which require employers to provide information to the IRS about the health plan coverage they offer (or do not offer) to their employees. The additional reporting is intended to promote transparency with respect to health plan coverage and costs. It will also provide the government with information to administer other ACA mandates, such as the large employer shared responsibility penalty and the individual mandate.
The Affordable Care Act (ACA) imposes significant information reporting responsibilities on employers starting with the 2015 calendar year. Employers with 50 or more full time equivalent employees (FTEs), as well as certain employers with fewer than 50 FTEs are subject to the new reporting requirements as of January 1, 2016. The ACA added two new sections to the Internal Revenue Code, Sections 6055 and 6056, which require employers to provide information to the IRS about the health plan coverage they offer (or do not offer) to their employees. The additional reporting is intended to promote transparency with respect to health plan coverage and costs. It will also provide the government with information to administer other ACA mandates, such as the large employer shared responsibility penalty and the individual mandate.
In light of the complexity of the new ACA information reporting requirements, employers should consider taking the following actions now:
- Learn about the new information reporting requirements mandated by the Affordable Care Act.
- Determine which (if any) of the ACA reporting requirements your organization is subject to.
- Review ownership structures of related companies and perform a controlled/affiliated service group analysis to determine whether or not your company is considered an Applicable Large Employer under the ACA (a so-called ALE )
- Review the instructions for Forms 1094-C and 1095-C and, if applicable, the instructions for Forms 1094-B and 1095-B, along with the forms
- Develop procedures for determining and documenting each employee’s full-time or non-full-time status by month
- Develop procedures to collect information about offers of health coverage and health plan enrollment by month
- Ensure that systems are in place during 2015 to collect the needed data for the forms
ACA guidance from Waugh Agency, LLC – “Innovative service, Genuine Attention”
 We understand the technical components of the ACA, and we are prepared to counsel you on upcoming required healthcare changes and new options and requirements for health plans. Allow us to help you develop a customized ACA compliance program for your business. Call Waugh Agency, LLC at 413-527-2738.
We understand the technical components of the ACA, and we are prepared to counsel you on upcoming required healthcare changes and new options and requirements for health plans. Allow us to help you develop a customized ACA compliance program for your business. Call Waugh Agency, LLC at 413-527-2738.
Secure, Fast, Trusted.
Simply complete the the following form, a licensed specialist will contact you. Or, call us at (800)779-4090.
ACA Information Reporting Quick Reference Chart
Whether or not your company is subject to ACA information reporting depends on the size of your company and the type of health insurance plan you offer (including offering no health insurance).
Refer to the chart below to determine if your company is subject to ACA Information Reporting:
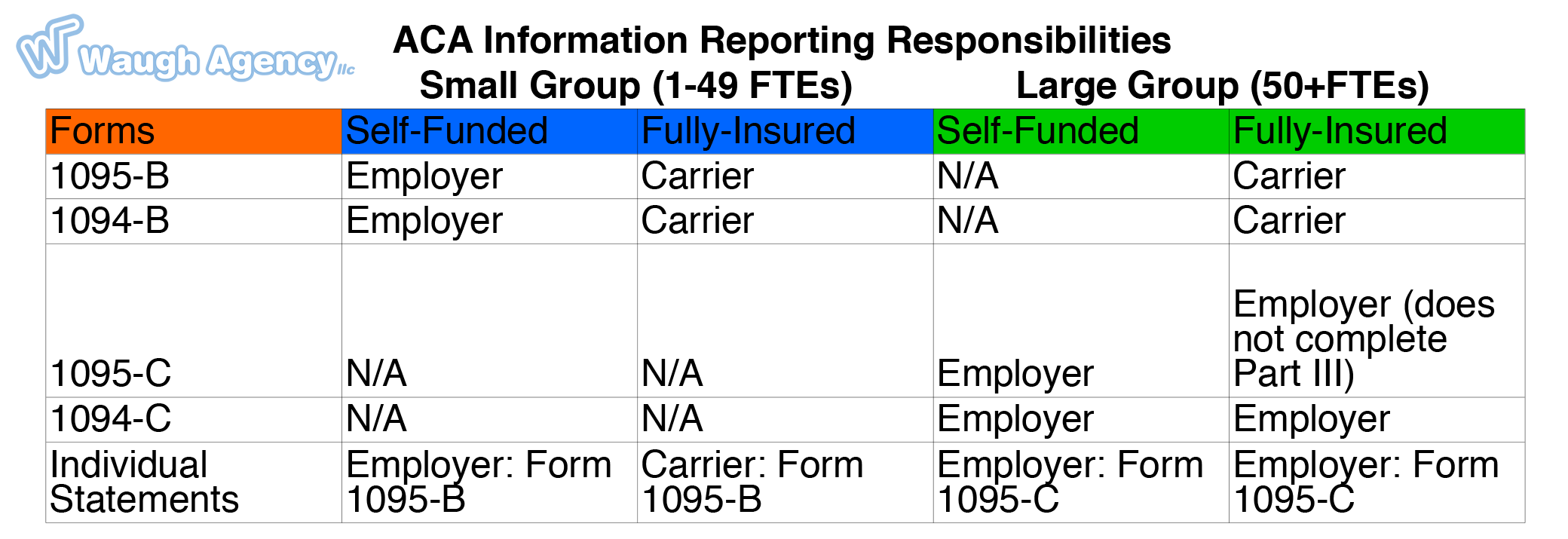
ACA Information Reporting for Small Group Self Funded Plans
As noted in the chart above, the only small groups (under 50 FTEs) subject to ACA information reporting are those with self funded health plans (see below for additional exception for controlled groups). Self-insured health plans will use Form 1095-B and Form 1094-B to report the name, address and Social Security number (or date of birth) of employees and their family members who have coverage under the self-insured plan. Employees who are offered coverage, but decline the coverage, are not reported.
Controlled Groups: majority owned companies are aggregated
Small employers with fewer than 50 full-time employees (including equivalents) will be required to file Forms 1095-C and 1094-C if they are members of a controlled or affiliated group that collectively has at least 50 full-time employees (including equivalents). Companies could be in a controlled or affiliated service group if they have common owners, provide services for each other or work together to provide services to third parties.
Example: Smith and Jones each own 50 percent of Company A and Company B. Because of this ownership, A and B are a controlled group, and the filing requirements for A and B are based on the number of employees that they have collectively. If A and B together had at least 50 full-time employees (including equivalents) in the prior calendar year, then A and B are each a member of an “applicable large employer group” for the current year, and both A and B would be required to file the forms. Thus, if A had 35 full-time employees in the prior calendar year and B had 30, A and B would each be a member of an applicable large employer group with 65 employees, and both would have to file Forms 1095-C and 1094-C. If A had 35 full-time employees and B had only 10, then A and B would not be members of an applicable large employer group since, collectively, they only had 45 employees (which is less than the 50-employee threshold). In that case, neither A nor B would file Forms 1095-C and 1094-C.
Secure, Fast, Trusted.
Simply complete the the following form, a licensed specialist will contact you. Or, call us at (800)779-4090.
ACA Information Reporting F.A.Q.’s:
Forms: There are 4 forms: 2 information returns (the 1095 series) and 2 transmittal forms (the 1094 series).
- 1095-B – Health Coverage
- 1094-B – Transmittal of Health Coverage Information Returns
- 1095-C – Employer Provided Health Insurance Offer and Coverage
- 1094-C – Transmittal of Employer Provided Health Insurance Offer and Coverage Information Returns
Overview of the information reporting process
The new ACA information reporting system is similar to the current Form W-2 reporting system in that an information return (Form 1095-B or 1095-C) will be prepared for each applicable employee, and these returns will be filed with the IRS using a single transmittal form (Form 1094-B or 1094-C). Electronic filing is required if the employer files 250+ returns. Employers must file these returns annually by Feb. 28 (March 31 if filed electronically). Therefore, employers will be filing these forms for the 2015 calendar year by Feb. 28 or March 31, 2016. A copy of the Form 1095, or a substitute statement, must be given to the employee by Jan. 31 and can be provided electronically with the employee’s consent. Employers will be subject to penalties of up to $200 per return for failing to timely file the returns or furnish statements to employees.
The filing requirements are based on an employer’s health plan and number of employees. Generally, only ALE’s are subject to ACA information reporting, see exceptions above for small employer self funded plans, and for controlled groups. ALEs are required to comply with ACA information reporting if they offer an insured or self-insured health plan, or even if they do not offer any group health plan.
Applicable large employers are those that had, on average, at least 50 full-time equivalent employees (FTE’s) during the preceding calendar year. For purposes of the ACA full time is considered >=30 hours/week, part time employees are aggregated.
How will the IRS use the information gathered?
The IRS will use the information submitted on the ACA information reporting forms to determine whether employees are subject to the new shared responsibility penalty for not having health coverage. The information will also allow the IRS to determine if an employer is liable for a shared responsibility penalty. These are the so-called “play or pay” penalties that were supposed to take effect in 2014, but were delayed in 2013 by the Obama administration.
The employer shared responsibility penalty can be imposed on any ALE that does not offer affordable, minimum value health coverage to all of its full-time employees. Health coverage is affordable if the amount that the employer charges an employee for self-only coverage does not exceed 9.5 percent of the employee’s Form W-2 wages, rate of pay, or the federal poverty level for the year. A health plan provides minimum value if the plan is designed to pay at least 60 percent of the total cost of medical services for a standard population. In the case of a controlled or affiliated service group, the penalties apply to each member of the group individually.
Penalty Relief for most employers in 2015, but reporting still required
ALEs with fewer than 100 FTEs are generally eligible for transition relief from the employer shared responsibility penalty for their 2015 plan year. Nonetheless, these employers are required to file Forms 1095-C and 1094-C for the 2015 calendar year.
Secure, Fast, Trusted.
Simply complete the the following form, a licensed specialist will contact you. Or, call us at (800)779-4090.
